|
|
Official Journal of the
|
ISSN: 1983-991X
|
|
| Case Report « PDF file » |
|
Laparoscopic Treatment of Gastric Trichobezoar
Felipe Cardoso Della Bidia, MD1; Pedro Bastos Guimarães de Almeida, MD1; Heleno Pinto de Moraes, Professor of Pathology, MD, PhD2; Marcos Filgueiras, Professor of Surgery, MD2; Ricardo Zorron, Professor of Surgery, MD, PhD3
1 Department of Surgery - University Hospital Teresopolis HCTCO - FESO, Rio de Janeiro- Brazil; 2 Chief of the Division of Pathology - University Hospital Teresopolis HCTCO - FESO, Rio de Janeiro- Brazil; 3 Chairman, Department of Surgery - University Hospital Teresopolis HCTCO- FESO, Rio de Janeiro- Brazil.
ABSTRACT
Trichobezoar is a mass of swallowed hair that accumulates in the stomach and fails to pass through the intestines.
They occur in young patients, typically female with mental
disorders. Many approaches have been proposed for the
treatment of bezoars, such as gastroscopic fragmentation, nasogastric lavage or suction, enzymatic therapy, and laparotomy.
With the advent of laparoscopic surgery, it became possible to remove such lesions without large abdominal incisions,
better cosmetics and reduced pain. The aim of the study is to present an 18-year-old female who had gastric trichobezoar
that was successfully treated with a laparoscopic technique, using anterior gastrotomy and laparoscopic suture.
The laparoscopic approach may be the treatment of choice for trichobezoar removal in the future, with potential benefits to
the patients.
Key words: Trichobezoar, laparoscopic surgery, laparoscopy, minimally invasive surgery, gastric surgery.
Bras. J. Video-Sur, 2008, v. 1, n. 4: 178-181
| Accepted after revision: August, 05, 2008. |
INTRODUCTION
he Word bezoar means antidote and is derived
from three words: from the Arabic
"badzher", from the Persian "padzhar" and from the
Hebrew "beluzaar". In the XII century it was believed
that bezoars obtained from animals held curative
properties and they were used to treat bites of snakes
and intoxication1.
Nowadays, bezoars are defined as an agglomeration of foreign material in the intestinal
tract, usually they are found in the stomach; however,
they may extend until the small intestine or
present fragmentation with multiple mass in any segment
of the intestine2. Bezoars are classified in 4
categories: phytobezoars (vegetable matter); trichobezoars
(hair balls); pharmacobezoars (tablets or semi-liquid
masses drugs); miscellaneous material (clay, stone
etc…)3.
Trichobezoars are composed by fragments of swallowed hair (trichophagia) and it is called
Rapunzel Syndrome when it extends through the pylorus
2. Trichobezoars represent 55% of human bezoars, it
is more frequent in women (90%) and approximately 80% of the patients are less than 40 years
old. Trichobezoars typically occur in female
patients younger than 30 years with mental
disorders. Triggering etiologic factors such as inadequate
diet, ingestion fiber or poor mastication, habits
and psychological disorders; 40 % of the cases are associated with psychiatric
disorder1.
Conventional gastrotomy was the treatment of choice in case of obstruction, but nowadays
the laparoscopic approach is a feasible technique to
treat patients with this disease.
CASE REPORT
An 18-year-old Caucasian Brazilian female patient, a single student from Nova Iguaçu, was admitted at the emergency service of the Hospital das Clínicas de Teresópolis- HCTCO with complaints of severe epigastric pain for the last 6 months, associated with nausea and eventual vomiting. The patient reported weight loss in the last month. The patient was lucid, well-oriented, anxious, hydrated, pale +2/+4; non-cyanotic, afebrile, eupneic, absence of cervical palpable lymph nodes. The physical examination of the abdomen revealed absence of audible peristalsis, hernias; at percussion it was observed a tympanic note in the right upper and lower quadrants and dullness in the left upper and lower quadrants. Presence of painful palpation with a homogeneous mass in the epigastrium is noticed. Bowel sounds were present on auscultation. Upper digestive endoscopy showed a trichobezoar with the shape of the stomach that extended until the antrum, although the visibility was compromised, the endoscope passed through the gastric pouch. Pylorus was mobile, centered and pervious. Laparoscopy was the treatment of choice and the patient was submitted to the surgery under general anesthesia.
OPERATIVE TECHNIQUE
Four trocars were placed under direct vision: umbilicus (10mm), left flank (5mm), and two
trocars in the right flank (10mm, 5mm). Hasson's
technique was used to insert the first trocar with insufflation
of CO2 at 12mmHg pressure. Laparoscopic
gastrotomy using hook was performed with an 8 to 10cm
longitudinal incision on the gastric antrum region. As
the bezoar had a hard consistency and occupied the
whole gastric cavity, it was difficult to mobilize it.
The trichobezoar was removed from the stomach and
the highly contaminated specimen was immediately isolated in a bag. Gastrostomy was closed with
a contiguous 3.0 polypropylene suture and the
specimen retrieved in a plastic bag (Figure1-4),
extending umbilicus trocar incision. The patient had a
good postoperative recovery. An infection on the
operative wound was treated with the withdrawal of
the bandage and local wound care, the patient
deambulated on the 2º postoperative day and on the 3º
postoperative day the patient accepted well the eating diet. On
the 4º postoperative day the patient was discharged
from hospital after a psychiatric evaluation. After 6
months follow-up there was no case of recurrence.
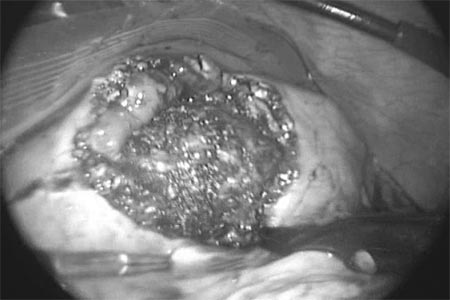 |
Figure 1 -Laparoscopic image of gastrotomy on the gastric
antrum and visualization of the trichobezoar. |
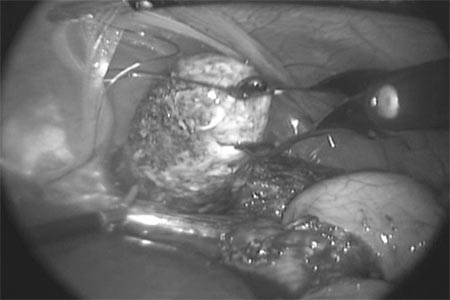 |
Figure 2 -Trichobezoar removal with immediate isolation in
a bag. |
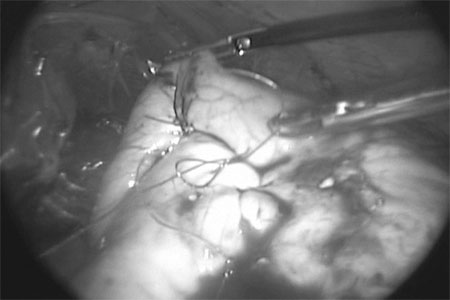 |
Figure 3 -Gastrotomy closure with contiguous 3.0
polypropylene suture. |
 |
Figure 4 -Surgical specimen. |
DISCUSSION
The first authentic case of human trichobezoar was described in
17794, thus in 1995 Filipi et
al5 reported a per-oral removal of trichobezoars. Typical symptoms are
palpable epigastric mass (that frequently assume the
shape of the stomach) accompanied with pain,
nausea, vomiting, and weight loss, hematemesis may
occur. Presence of symptoms depends on the evolution,
the elasticity of the stomach and the size of the
bezoar. Complications include ulcers (with or
without bleeding), perforation, intussusception and
obstruction, usually in the terminal ileum; malnutrition is a
frequent accompaniment 6. The analysis of these data
in addition to the anamnesis can indicate the
diagnosis; however, at the beginning of the consultation
the majority of the patients deny
trichophagy1.
Abdominal radiograph is of limited use in patients with trichobezoar; the upper
gastrointestinal tract barium study, which is indicated to
diagnosis differentiation of epigastric masses, is a highly
sensitive and specific examination. Other exams with
excellent specificity are: ultrasound which detects
trichobezars as mobile hyperechoic mass with acoustic
shadowing; endoscopy can directly reveal a ball of hair;
however it is not able to anatomically define the extension
of the lesion; and computed tomography(CT) with
similar diagnostic indexes to the upper gastrointestinal
tract contrast exam 2 showing a well-defined
intraluminal heterogeneous mass with interspersed gas in
its interstices7, CT best describes the size,
configuration and location, besides it differentiates trichobezoars
from neoplasms4.
The treatment of a bezoar may be conservative for small bezoars with the use of
methods such as enzymatic and prokinetic; endoscopic
(more valuable for phytobezoar); electrohydraulic
lithotripsy; laparotomic or laparoscopic surgery
3. Some cases of spontaneous resolution of gastric bezoars have
been described in the literature8.
Although there are some methods for the treatment of bezoars, in the case of
trichobezoars the enzymatic dilution is not possible and
endoscopic retrieval is difficult due to the extension of the
mass, which is difficult to be
fragmented4. The endoscopic treatment represents extra risks of
gastric perforation and posterior bowel obstruction due
to the advance of fragments through the digestive tract.
The supraumbilical laparotomic surgery allows through gastrotomy a direct and fast
approach; however, the most frequent complication is
the bacterial contamination, due to patient malnutrition
it may lead to severe peritonitis 9 besides it can
not eliminate the immediate postoperative
inconvenience of this approach, mainly the cicatricial sequelae of
longitudinal abdominal incisions.
Nowadays the laparoscopic approach has been used with success in a great number of
abdominal surgeries with significant shorter operative
time, less postoperative complications and reduced
hospital stay10. The great outcome achieved with our
patient proves the feasibility and safety of the method,
which is similar to the conventional approach. The
initial reports about the use of this approach to
remove gastrointestinal bezoars are potentially
advantageous and this alternative may be suggested as the
treatment of choice 11,12. After surgery, patients should have
an adequate neuropsychiatric follow-up in order to
avoid recurrences.
REFERENCES
1. Ruiz HD, Palermo M, Ritondale O, Pest E, Pest P,
Villafañe V, Bruno M, Tarsitano FJ. Tricobezoares
gastroduodenales: una causa poco frecuente de obstrucción del tracto de
salida. Acta gastroenterol latinoam ; 35(1):24-27, 2005.
2. Jesus Lisieux Eyer de, Novelli Rosa JM. Trichobezoar.
Rev. Col. Bras. Cir. 2005; 32(3):157-160.
3. Bartolomucci AC, Marotta A, Santos EM.
Gastric-duodenum-jejune trichobezoar:
videolaparoscopic management. Rev. Col. Bras. Cir.
2004 ;31(3):215-216.
4. Palanivelu C,Rangarajan M,Senthilkumar
R,Madankumar MV. Trichobezoars in the stomach and ileum and
their laparoscopy-assisted removal: a bizarre case. Singapore
Med J. 2007 Feb; 48 : 37-39
5. Filipi CJ, Perdikis G, Hinder RA, DeMeester
TR, Fitzgibbons RJ Jr, Peters J. An intraluminal surgical
approach to the management of gastric bezoars. Surg Endosc
1995 Jul;9(7):831-3
6. Jiledar J, Singh G, Mitra SK. Gastric perforation
secondary to recurrent trichobezoar. Indian J Pediatr. 1996;
63(5):689-91.
7. M J O'Sullivan, G McGreal, J G Walsh, and H P
Redmond. Trichobezoar. R Soc Med. 2001 February; 94(2): 68_70.
8. Kadian RS,Rose JF,Mann NS. Gastric
bezoars—spontaneous resolution. Am J Gastroenterol. Vol. 70.
1978 Jul; 79-82.
9. Baeza HC, Franco VR. Tricobezoar gástrico y el
síndrome de Rapunzel. Bol Med Infant Mex 1987; 44:167-171
10. Yau KK,Siu WT,Law BK,Cheung HY,Ha JP,Li
MK. Laparoscopic approach compared with conventional
open approach for bezoar-induced small-bowel obstruction.
Arch Surg . Vol 140, ed 10. 2005 Oct: 975-975.
11. Nirasawa Y, Mori T, Ito Y, Tanaka H, Seki N, Atomi
Y. Laparoscopic removal of a large gastric trichobezoar. J
Pediatr Surg 1998; 33:663 _ 5.
12. Yao CC, Wong HH, Chen CC, Wang CC, Yang CC,
Lin CS. Laparosopic removal of large gastric
phytobezoars. Surg Laparosc Endosc Percutan Tech 2000; 10:
243-245.
Correspondence address:
Felipe Della Bidia
Rua Cel. Manoel Martins Jr., 730
Jardim Esplanada 2
São José dos Campos, SP - Brazil
CEP: 12242-810
Email: felipedellabidia@hotmail.com
